Endoscopic Sinus and Nasal Surgery
Endoscopic Sinus and Nasal Surgery
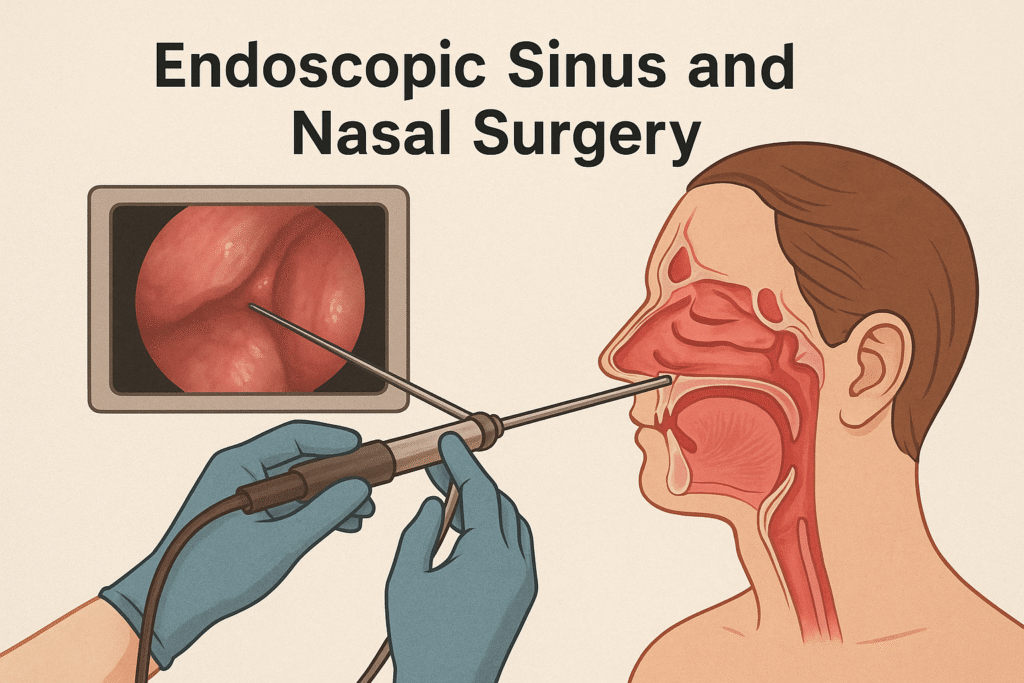
Endoscopic sinus and nasal surgery, also known as Functional Endoscopic Sinus Surgery (FESS), is a minimally invasive technique used to restore proper drainage and function of the paranasal sinuses. It has become the gold standard for treating chronic rhinosinusitis (CRS), nasal polyposis, and other sinonasal pathologies unresponsive to medical management.
This surgical advancement allows otolaryngologists to work through the nostrils without external incisions, using an endoscope to provide magnified visualization of the nasal cavity and sinus anatomy.
Anatomy of the Paranasal Sinuses
The paranasal sinuses are air-filled spaces within the bones of the face and skull. They include:
Maxillary sinuses (cheek area)
Frontal sinuses (forehead)
Ethmoid sinuses (between the eyes)
Sphenoid sinuses (behind the nose)
These sinuses are connected to the nasal cavity through narrow channels. Blockage of these passages can lead to infection, inflammation, and chronic sinusitis.
Indications for Surgery
Endoscopic sinus surgery is considered when conservative treatments fail, including:
Chronic rhinosinusitis (with or without nasal polyps)
Acute recurrent sinus infections
Obstructive nasal polyposis
Mucoceles
Sinus fungal infections
Deviated nasal septum obstructing sinus outflow
Sinus tumors (benign or malignant)
Cerebrospinal fluid (CSF) leaks
Preoperative Evaluation
A thorough assessment is crucial for optimal outcomes:
History & Physical Examination: Including nasal endoscopy
Imaging: High-resolution CT scan of the sinuses to evaluate extent of disease
Medical therapy trial: At least 6–12 weeks of intranasal corticosteroids, nasal irrigation, and antibiotics (if indicated)
Surgical Technique
1. Anesthesia
Typically performed under general anesthesia
Local anesthesia may be used in select cases
2. Endoscopic Access
A rigid endoscope (usually 4mm in diameter) is introduced through the nostril
Nasal decongestants and local vasoconstrictors are used to reduce bleeding
3. Surgical Steps
Removal of diseased mucosa, polyps, or bony partitions
Widening of the natural sinus ostia
Preservation of mucosa when possible
Navigation assistance (image-guided surgery) may be used in complex anatomy
Advantages
No external scars
Improved sinus ventilation and drainage
Faster recovery time
Reduced hospital stay
Better preservation of normal structures
Postoperative Care
Nasal saline irrigations (several times daily)
Topical or systemic corticosteroids
Antibiotics if infection is suspected
Avoidance of strenuous activity for 2 weeks
Regular follow-up with debridement if necessary
Potential Complications
While generally safe, risks include:
Bleeding (epistaxis)
Orbital injury (rare)
CSF leak
Adhesions (synechiae)
Altered sense of smell
Recurrent polyps or sinusitis
Outcome & Prognosis
Endoscopic sinus surgery has a high success rate when performed on appropriate candidates. Most patients report significant improvement in quality of life, reduced infection rates, and improved nasal breathing. Long-term management may still require maintenance therapy, especially in patients with polyps or allergies.